In-vitro gametogenesis shows promise for many infertile couples, but scientists have warned of ethical issues. In past decades, the field of reproductive medicine has witnessed huge advances.

Scientists have gained a better understanding of embryonic development, have refined their use of fertility treatments and have come up with revolutionary techniques to identify and prevent disease in babies – the so-called "three-DNA babies" is perhaps the greatest example.
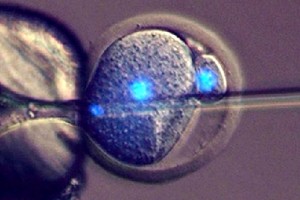
However, some of these advances are also causing a number of ethical concerns that scientists and lawmakers will have to address in the coming years. This is the case of a revolutionary technique thus far successful in mice and known as in-vitro gametogenesis (IVG). The method is redefining the notion of what is possible in reproductive and regenerative medicine, as it opens up the possibility of creating human sperm and eggs from induced pluripotent stem cells.
"It is hard to predict when innovative fertility technologies will be ready for use in humans. Ten years ago, we didn't think that egg freezing would arrive so quickly but it did. We just don't know when in-vitro gametogenesis will be used in humans, but the fact that it has been done successfully in mice makes is very interesting - if fertility treatments work in mice they usually end up working in humans at a later stage", Joyce Harper, professor of human genetic and embryology and Deputy Chair on the board of the the British Fertility Society told IBTimes UK.
IVG could potentially help couples with certain types of infertility and advance our basic knowledge of how gametes are formed and of inherited diseases. But this comes with a range of scientific and ethical questions that scientists from Harvard and Brown University have summed up, in a new article published in Science Translational Medicine.
IVG is defined as the generation of eggs and sperm from pluripotent stem cells derived from adult body tissues, such as skin cells. This may lead to the creation of embryos from these gametes. Although IVG's attempts in human and nonhuman primates have so far been unsuccessful, the authors point out that studies in mice have already illustrated the immense opportunities brought by this technique.
The first is that it could answer basic science questions by allowing researchers to learn more, at a molecular and cellular level, about sperm and egg formation, about development, but also about genetic diseases. In a more distant future, it could also greatly improve current reproductive techniques and help a greater number of infertile couples. It could, for example, benefit cancer survivors who have undergone chemotherapy and have lost reproductive function as a result.
It may also eliminate the need for egg donors and help women who don't naturally produce functional eggs. Some have argued that this would pave the way for same-sex couples to conceive, using both of the parents' genetic material, but this is still a long way away. Older women may also find it easier to become mothers. "The number of women delaying pregnancy is growing and around the world the age of first-time mothers is increasing. For some older women, it can be difficult to conceive using their own eggs, and this new technique could help them and be very important in accompanying this trend. Of course this comes with a set of ethical questions - will we see more and more women starting a family in their 40's or 50's?", Harper pointed out.
IVG could also help refine current IVF procedures and make them less uncomfortable for women. Indeed, the technique would allow for an easy and rapid creation of many eggs from stem cells, rendering the need to stimulate the hormone of women to retrieve their own eggs unnecessary. However, the article emphasises that the technique could also be risky, and important ethical considerations must be taken into account.
The most important concern – although it is probably the most far-fetched – is that this technique could one day lead to the emergence of "designer babies". Because IVG would allow for the generation of many gametes and many embryos cheaply, parents would have more chances to choose the embryo they want to implant, to have their "ideal baby". The authors write: "Of course, successfully using the technology in this way would require far deeper knowledge of human genetics than we currently have. Nevertheless, even at this stage, it is worth contemplating the ethical issues raised by such a possible future, which would directly force regulators to make difficult decisions on drawing the line between alterations that end harmful conditions versus eugenics."
Having the possibility to create many embryos would surely allow embryonic research to progress, but it would receive the opposition of many, on moral or religious grounds. Indeed, it potentially opens the door to the practice of "embryo farming". "IVG may raise the spectre of 'embryo farming' on a scale currently not imagined, which might exacerbate concerns about the devaluation of human life", the scientists add.
Of more immediate concern howeveris whether this technique will be really safe to use in humans. It will be necessary to study its full impact on the long-term health of any offspring generated. Large and robust clinical trials will therefore have to be conducted before any use of IVG in humans is allowed.
Quelle: International Business Times
